How to Coordinate Care When Everyone Is Juggling Too Much

Caring for someone rarely happens in isolation. It unfolds alongside full-time jobs, parenting, long commutes, medical appointments, and the quiet mental load of daily life. Most families don’t struggle with care because they don’t care enough. They struggle because aligning people, information, and decisions across busy schedules is genuinely hard.
When coordinated care breaks down, it usually isn’t due to neglect or indifference. It’s due to missed updates, unclear roles, and systems that rely too heavily on one person to keep everything straight. This article focuses on realistic ways families and care teams can build coordination that fits into real life. Not perfect systems. Not constant meetings. Just practical approaches that reduce stress and help everyone stay aligned.
What Coordinated Care Really Means
At its simplest, coordinated care means that care efforts are aligned rather than fragmented. Information flows in a way that makes sense. Decisions don’t get lost between people. Everyone involved has a shared understanding of priorities, even if they’re not involved in every detail. In real family settings, coordinated care often looks less formal than it sounds. It might mean siblings can see appointment updates without asking, or a care team knows who to contact and when. These systems don’t remove responsibility, but they distribute it more evenly.
Another important distinction is between helping and coordinating. Helping is often reactive, stepping in when something goes wrong or when someone asks. Coordination is proactive. It anticipates needs and reduces the likelihood of last-minute stress or confusion.
What often gets overlooked is that coordination creates emotional safety. When people know there is a shared plan and a reliable way to stay informed, they are less likely to second-guess decisions or worry that something important is happening without them. This sense of predictability is especially important in care situations where uncertainty is already high.
Why Full Schedules Make Coordination So Hard
Most people involved in caregiving are already managing competing demands. Work responsibilities, parenting, financial pressures, and personal health all require attention. Adding care coordination on top of that can feel like one responsibility too many. Information overload is a major contributor. Updates come through texts, calls, emails, and conversations that happen when not everyone is present. Over time, important details get missed or repeated, and people stop feeling confident they know what’s going on.
Emotional fatigue also plays a role. When stress is high, decision-making becomes harder and communication can feel heavier than it needs to be. Even well-intentioned people can unintentionally create gaps simply because there’s too much to manage at once.
Over time, this fatigue can change behavior. People delay responding, avoid conversations that feel complex, or assume someone else will handle it. Without coordinated care systems in place, these small coping strategies quietly undermine alignment and increase the risk of misunderstandings.
The Hidden Cost of Poorly Coordinated Care
When coordination falters, the impact is felt quickly. Families may experience constant low-level anxiety, unsure whether something important has been overlooked. Caregivers may duplicate work or give inconsistent information without realizing it.
Routines can become unstable, especially for those receiving care. Small disruptions add up, affecting comfort, trust, and overall well-being. What feels like a minor miscommunication to one person may feel unsettling to another.
Over time, communication can become reactive. Instead of steady updates, families hear only when something goes wrong. This pattern erodes trust and increases stress, even when everyone involved is doing their best. This reactive pattern can also affect decision-making quality. When updates arrive late or without context, families are forced to respond quickly with limited information. Coordinated care helps shift communication from crisis-driven to continuity-driven, improving both confidence and outcomes.
Who Usually Ends Up Coordinating Care (And Why That’s a Problem)
In many families, one person quietly becomes the default coordinator. This might be the adult child who lives closest, the sibling who is most organized, or the person who tends to respond first. While this arrangement can feel efficient at first, it often leads to imbalance. That person carries the mental load of remembering details, relaying updates, and anticipating needs, often without support.
True coordinated care relies less on one person’s capacity and more on shared visibility. When information is accessible and responsibilities are clear, coordination becomes a shared structure rather than a personal burden. Shared visibility also reduces tension within families. When everyone can see what is happening, assumptions decrease, and conversations become more constructive. Instead of debating whether enough is being done, families can focus on how to support one another effectively.
The Role of a Patient Care Coordinator
A patient care coordinator exists to reduce care fragmentation. This role focuses on aligning information, supporting communication, and helping ensure continuity across people and settings. In formal healthcare environments, this may include scheduling, follow-ups, and care planning. In family situations, coordination often happens informally, without clear boundaries or tools.
Understanding what a patient care coordinator does can help families replicate parts of that role. The goal isn’t to professionalize family care, but to adopt coordination practices that reduce stress and improve clarity. Even small elements of this role can make a difference. Tracking decisions, clarifying next steps, and ensuring updates reach the right people are all coordination functions that support continuity. These practices help families move from reacting to managing care more intentionally.
Practical Ways to Coordinate Care With Limited Time
Effective coordination doesn’t require endless meetings or constant messages. It starts with centralizing information, so updates live in one reliable place rather than scattered across conversations. Clear expectations around communication also help. Knowing when updates will be shared and how urgent matters are handled reduces anxiety and interruptions.
Shared tools can replace memory and long text threads. When information is documented once and visible to those who need it, coordination becomes more consistent and less exhausting. This approach also reduces the emotional pressure on caregivers to be constantly available. Coordinated care systems allow people to engage when they have capacity, without fearing that stepping away will cause something to fall apart.
How to Divide Responsibilities Without Creating More Work
Dividing responsibilities works best when roles are realistic and clearly defined. Assigning tasks based on strengths and availability helps avoid resentment and confusion. Vague roles often create more work than they solve. When no one knows who owns a task, follow-ups multiply, and stress increases.
Simple ownership, even for small responsibilities, supports smoother coordinated care and helps everyone feel confident about what they’re responsible for. Clear ownership also makes it easier to adjust when circumstances change. If someone becomes unavailable, tasks can be reassigned intentionally instead of disappearing. This flexibility is key to maintaining coordination over time.
Coordinated Care Across Distance and Different Schedules
Distance adds complexity, but it doesn’t make coordination impossible. Families across time zones often rely on asynchronous communication to stay aligned. Regular summaries and documented updates help people stay informed without being present in real time. This approach respects different schedules while maintaining connection.
The goal isn’t constant communication. It’s a shared understanding that holds up even when people are unavailable. When families prioritize shared understanding, communication becomes more efficient and less emotionally charged. People can trust the system rather than rely on constant check-ins to feel informed.
Building Coordination That Holds Up During Stressful Moments
Stressful moments quickly reveal weaknesses in coordination. Emergencies, health changes, and transitions require clarity more than speed. Preparing systems in advance makes these moments easier to navigate. Documented contacts, decision roles, and communication plans reduce panic.
When coordination holds up under pressure, families feel supported rather than overwhelmed. This support is not just logistical but emotional. Clear coordination reassures families that they are not facing uncertainty alone, even during high-stress moments when quick decisions are required.
How Care Communities Can Support Coordinated Care
Care communities play a critical role in supporting coordinated care. Consistent communication and transparency reduce uncertainty for families. When care teams provide predictable updates and clear next steps, families feel included rather than reactive.
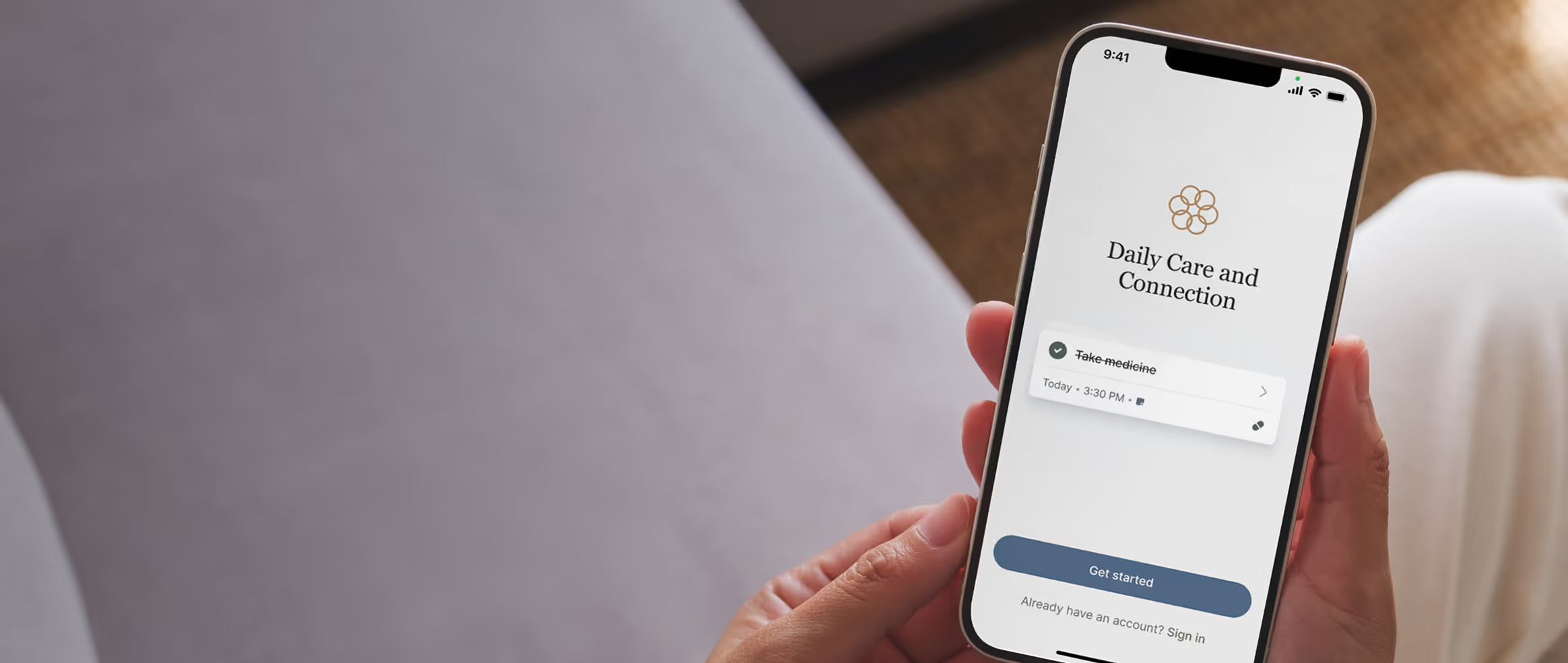
Tools like Caily can support this work by offering a shared space for communication and coordination without adding complexity. When care communities and families use shared systems, trust builds more naturally. Families feel informed, care teams feel supported, and coordination becomes a stabilizing force rather than another task to manage.
What Coordinated Care Looks Like When It’s Working
When coordination works well, care feels steadier. Families experience fewer last-minute scrambles and less confusion. Communication becomes calmer and more predictable. People trust they’ll be informed without having to chase updates.
This steadiness creates emotional relief and allows everyone to focus on support rather than logistics. Over time, this shift improves relationships. When fewer conversations are spent clarifying or correcting information, more space is created for meaningful connection and thoughtful decision-making.
Moving Forward With Sustainable Coordination
Sustainable coordinated care develops over time. It evolves as needs change and relationships shift. Small, intentional improvements are often more effective than sweeping changes. Even a modest structure can make a meaningful difference. Coordination grounded in clarity and shared responsibility is more resilient and less likely to lead to burnout.
Families who invest in sustainable coordination often find that care feels less overwhelming, even as needs increase. The work doesn’t disappear, but it becomes more manageable, more humane, and easier to sustain.
Frequently Asked Questions About How to Coordinate Care When Everyone Is Juggling Too Much
What is coordinated care in everyday family situations?
In daily life, coordinated care means sharing information, responsibilities, and expectations clearly so care doesn’t rely on one person’s memory or availability.
How does a patient care coordinator help families?
A patient care coordinator helps align communication, schedules, and care plans so families and care teams stay on the same page.
Can coordinated care work if family members live far apart?
Yes. With shared tools and clear communication expectations, coordinated care can work effectively across distance and time zones.
What tools help support coordinated care?
Tools that centralize information and support shared visibility reduce confusion and improve continuity.

Get Started Now
Enjoy full access to everything Caily offers, from medication tracking to shared schedules and daily check-ins. See how much easier caregiving can be when everything is coordinated in one place.
Start your free trial